 Your new post is loading...
 Your new post is loading...
Depuis le 10 février 2019, la téléexpertise permet à un médecin de solliciter l’avis d’un confrère face à une situation médicale donnée. Ouverte dans un premier temps à certaines catégories de personnes, elle pourrait s’élargir d'ici fin 2020 à tous les patients.
Via IZYCARDIO
Conclusions: A telemedicine-based symptom reporting program facilitated early treatment of symptoms and improved lung function and functional status.
Background: Patients with chronic obstructive pulmonary disease (COPD) may not recognize worsening symptoms that require intensification of therapy. They may also be reluctant to contact a healthcare provider for minor worsening of symptoms. A telemedicine application for daily symptom reporting may reduce these barriers and improve patient outcomes.
Materials and Methods: Patients hospitalized for a COPD exacerbation within the past year or using supplemental O2 were approached for participation. Patients received optimal COPD care and were given a telecommunication device for symptom reporting. Initial symptom scores were obtained while patients were in their usual state of health. Patients were randomly assigned to an intervention group or a control group (usual medical care). The control group patients were instructed to seek medical care if their condition worsened. The intervention group symptom scores were assessed by a computer algorithm and compared with initial values. Scores 1 or more points above the initial score generated an “alert,” and patients were reviewed by a nurse and referred to a physician who prescribed treatment. Results: Eighty-six patients were screened; 79 met entry criteria and were randomized (intervention group, n=39; control group, n=40). Twelve patients submitted five or fewer symptom reports (5 intervention; 7 control) and were excluded from the analysis. Daily peak flow and dyspnea scores improved only in the intervention group. There were no differences in hospitalization and mortality rates between groups. No serious adverse events were reported.
Via rob halkes
Background: Few studies have evaluated both the overall effect of ICU telemedicine programs and the effect of individual components of the intervention on clinical outcomes.
Methods: The effects of nonrandomized ICU telemedicine interventions on crude and adjusted mortality and length of stay (LOS) were measured. Additionally, individual intervention components related to process and setting of care were evaluated for their association with mortality and LOS.
Results: Overall, 118,990 adult patients (11,558 control subjects, 107,432 intervention group patients) from 56 ICUs in 32 hospitals from 19 US health-care systems were included. After statistical adjustment, hospital (hazard ratio [HR] = 0.84; 95% CI, 0.78-0.89; P < .001) and ICU (HR = 0.74; 95% CI, 0.68-0.79; P < .001) mortality in the ICU telemedicine intervention group was significantly better than that of control subjects. Moreover, adjusted hospital LOS was reduced, on average, by 0.5 (95% CI, 0.4-0.5), 1.0 (95% CI, 0.7-1.3), and 3.6 (95% CI, 2.3-4.8) days, and adjusted ICU LOS was reduced by 1.1 (95% CI, 0.8-1.4), 2.5 (95% CI, 1.6-3.4), and 4.5 (95% CI, 1.5-7.2) days among those who stayed in the ICU for ≥ 7, ≥ 14, and ≥ 30 days, respectively. Individual components of the interventions that were associated with lower mortality, reduced LOS, or both included (1) intensivist case review within 1 h of admission, (2) timely use of performance data, (3) adherence to ICU best practices, and (4) quicker alert response times.
Conclusions: ICU telemedicine interventions, specifically interventions that increase early intensivist case involvement, improve adherence to ICU best practices, reduce response times to alarms, and encourage the use of performance data, were associated with lower mortality and LOS.
Via rob halkes
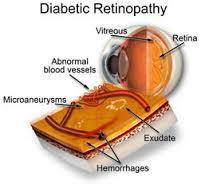
From "Telemedicine and e-Health" Comparing the Effectiveness of Telemedicine and Traditional Surveillance in Providing Diabetic Retinopathy Screening Examinations: A Randomized Controlled Trial To cite this article:
Steven L. Mansberger, Ken Gleitsmann, Stuart Gardiner, Christina Sheppler, Shaban Demirel, Kathleen Wooten, and Thomas M. Becker. Telemedicine and e-Health. December 2013, 19(12): 942-948. doi:10.1089/tmj.2012.0313. Published in Volume: 19 Issue 12: December 4, 2013
Abstract Objective: To determine the effectiveness of telemedicine for providing diabetic retinopathy screening examinations compared with the effectiveness of traditional surveillance in community health clinics with a high proportion of minorities, including American Indian/Alaska Natives. Subjects and Methods: We conducted a multicenter, randomized controlled trial and assigned diabetic participants to one of two groups: (1) telemedicine with a nonmydriatic camera or (2) traditional surveillance with an eye care provider. For those receiving telemedicine, the criteria for requiring follow-up with an eye care provider were (1) moderate nonproliferative diabetic retinopathy or higher, (2) presence of clinically significant macular edema, or (3) “unable to grade” result for diabetic retinopathy or macular edema. Results: The telemedicine group (n=296) was more likely to receive a diabetic retinopathy screening examination within the first year of enrollment compared with the traditional surveillance group (n=271) (94% versus 56%, p<0.001). The overall prevalence of diabetic retinopathy at baseline was 21.4%, and macular edema was present in 1.4% of participants. In the telemedicine group, 20.5% would require further evaluation with an eye care provider, and 86% of these referrals were because of poor-quality digital images. Conclusions: Telemedicine using nonmydriatic cameras increased the proportion of participants who obtained diabetic retinopathy screening examinations, and most did not require follow-up with an eye care provider. Telemedicine may be a more effective way to screen patients for diabetic retinopathy and to triage further evaluation with an eye care provider. Methods to decrease poor quality imaging would improve the effectiveness of telemedicine for diabetic retinopathy screening examinations.
[See download of complete article]
Via rob halkes
By Craig M. Lilly, MD; John M. McLaughlin, PhD, MSPH; Huifang Zhao; Stephen P. Baker, MScPH, (abd); Shawn Cody, RN, MSN, MBA; Richard S. Irwin, MD; on behalf of for the UMass Memorial Critical Care Operations Group Abstract Background Few studies have evaluated both the overall effect of intensive care unit (ICU) telemedicine programs and the effect of individual components of the intervention on clinical outcomes. Methods The effects of non-randomized ICU telemedicine interventions on crude and adjusted mortality and length of stay (LOS) were measured. Additionally, individual intervention components related to process and setting of care, were evaluated for their association with mortality and LOS. Results Overall, 118,990 (11,558 control; 107,432 intervention) adult patients from 56 ICUs in 32 hospitals from 19 US health care systems were included. After statistical adjustment, hospital (HR=0.84, 95%CI: 0.78-0.89, p<.001) and ICU (HR=0.74, 95%CI: 0.68-0.79, p<.001) mortality in the ICU telemedicine intervention group was significantly better than that of controls. Moreover, adjusted hospital LOS was reduced, on average, by 0.5 (95%CI: 0.4-0.5), 1.0 (95%CI: 0.7-1.3), and 3.6 (95%CI: 2.3-4.8) days, and adjusted ICU LOS was reduced by 1.1 (95%CI: 0.8-1.4), 2.5 (95%CI: 1.6-3.4), and 4.5 (95%CI: 1.5-7.2) days among those who stayed in the ICU for ≥7, ≥14, and ≥30 days, respectively. Individual components of the interventions that were associated with lower mortality and/or reduced LOS included: i) intensivist case review within 1 hour of admission, ii) timely use of performance data, iii) adherence to ICU best practices, and iv) quicker alert response times. Conclusions ICU telemedicine interventions, specifically interventions that increase early intensivist case involvement, improve adherence to ICU best practices, reduce response times to alarms, and encourage the use of performance data were associated with lower mortality and LOS.
Via rob halkes
|
"les Français arrivent tard à tout, mais enfin ils arrivent " (VOLTAIRE)
Via IZYCARDIO
Recognizing that licensing and regulation has not kept pace with the growth of telemedicine applications, a new report offers five recommendations for the successful adoption of telehealth. The recommendations, made by the Information Technology and Innovation Foundation, a District of Columbia-based think tank, include: Adoption of a standard definition for telehealth: While a recently published study found there to be seven different federal definitions of telehealth, the report's authors stress that H.R. 3750, the Telehealth Modernization Act of 2013, can remedy that "by defining telehealth to include healthcare delivered by real-time video, secure chat, secure email or telephone. ...Establishment of a single, national license for telehealth providers ...Creation of technology- and location-neutral insurance policies ...Collaboration by state prescription drug monitoring programs ...Funding of research to boost quality and lower costs of telehealth programs A framework for evaluating telehealth programs must consider socioeconomic aspects--not just the technological--argue researchers in an article published online recently in Telemedicine and e-Health. Costs, benefits, barriers and outcomes, including clinical outcomes, are among the integral socioeconomic factors at play in telehealth implementations, they say. Meanwhile, the American Telemedicine Association has suggested some changes to the Federation of State Medical Board's (FSMB) proposed regulation of telemedicine. Among the suggestions: Don't make remote consults more cumbersome than in-person treatment and clear the way for docs to practice across state lines.
To read more:
- read the report(.pdf)
Read more: 5 recommendations for telehealth success - FierceHealthIT http://www.fiercehealthit.com/story/5-recommendations-telehealth-success/2014-05-14#ixzz31slImddj
Via rob halkes, Marie Ennis-O'Connor
From "Telemedicoine and e-Health" Spanning Boundaries into Remote Communities: An Exploration of Experiences with Telehealth Chronic Disease Self-Management Programs in Rural Northern Ontario, Canada To cite this article:
Sara J.T. Guilcher, Tarik Bereket, Jennifer Voth, Vinita A. Haroun, and Susan B. Jaglal. Telemedicine and e-Health. December 2013, 19(12): 904-909. doi:10.1089/tmj.2013.0057. Published in Volume: 19 Issue 12: December 4, 2013
Abstract: Background: In rural and remote settings, providing education programs for chronic conditions can be challenging because of the limited access and availability of healthcare services. The purpose of this study was to explore the experiences of participants in a chronic disease self-management program via telehealth (tele-CDSMP) and to identify facilitators and barriers to inform future tele-CDSMP delivery models. Materials and Methods: Nineteen tele-CDSMP courses were delivered to 13 Northern Ontario (Canada) communities. Two types of group were delivered: (1) single telehealth site (one community formed a self-management group linked to program leaders via telehealth) and (2) multiple telehealth sites (several remote communities were linked to each other and program leaders via telehealth). Following the completion of the courses, participants were invited to partake in a focus group. Results: Overall, 44 people participated in the focus groups. Four main themes were identified by tele-CDSMP participants related to the overall experience of the program: (1) bridging the access gap, (2) importance of group dynamics, (3) importance of strong leaders, and (4) preference for extended session time. Key barriers were related to transportation, lack of session time, and access to Internet-based resources. The main facilitators were having strong program leaders, encouraging the development of group identity, and providing enough time to be comfortable with technology. Conclusions: Our findings suggest overall the tele-CDSMP was a positive experience for participants and that tele-CDSMPs are an effective option to increasing access to more geographically isolated communities.
[Se download of article]
Via rob halkes
Summary points Telehealthcare is personalised healthcare delivered over a distance; data are transferred from the patient to the professional, who then provides feedback In patients with severe long term conditions, such as problematic asthma and diabetes, telehealthcare can reduce hospital admissions without increasing mortality Potential pitfalls include user interface problems, technical problems, and safety concerns such as data loss and confidentiality Telehealthcare can alter the doctor-patient relationship so try to humanise the interaction Consider workflows, to minimise unintended disruptions to normal routines Careful assessment of effectiveness, cost effectiveness, and safety considerations is needed before introduction Telehealthcare is the provision of personalised healthcare over a distance.1 It has the three following essential components2w1: The patient provides data such as a voice recording, video, electrocardiography, or oxygen saturation that gives information about the illness. Information is transferred electronically to a healthcare professional at a second location. The healthcare professional uses clinical skills and judgment to provide personalised feedback tailored to the individual. Telehealthcare can be delivered by both synchronous and asynchronous (such as store and forward) technologies (fig 1⇓). For example, telephone and video conferencing enable consultations in real time. An example of asynchronous communication would be storing two weeks’ of spirometry results in a batch and forwarding these on to a healthcare provider, who responds by email or telephone. Telehealthcare is related to, but distinct from telemedicine, where technology is used to share information over a distance between healthcare providers.2 Why is interest in telehealthcare increasing? Healthcare systems globally are facing major challenges such as ageing populations, increasing numbers of people living with long term conditions, patients in remote areas or with limited mobility, and increasing expectations for patient centred healthcare.w2 w3 Telehealthcare offers potential solutions to these challenges (see box 1),3 but the acceptability and effectiveness, and the safety considerations associated with its adoption need careful consideration. Read the whole article1
Via rob halkes
A clear majority of both patients with chronic diseases and the health professionals who treat them are in favour of the remote monitoring of patients’ conditions, according to the first ever study in Spain of the practice conducted by the IESE...
Via rob halkes
|



 Your new post is loading...
Your new post is loading...

















La TELE-EXPERTISE ne peut pas fonctionner sans EXPERT... Chaque professionnel de santé a une expertise à partager. Son usage devrait concerner tous les professionnels de santé (infirmiers, pharmaciens, médecins...) et tous les patients